Complications from Implant Surgery
I wanted to start a discussion on this case. Many of you know this individual and she was going to be our patient in the upcoming Live Implant Seminar in May. A bit of background, this patient had an existing root canaled tooth on #7. Here is the preoperative clinical situation:
There was a vertical root fracture and the tooth was going to be lost. The patient had the tooth extracted and implant placed after a surgical guide was fabricated for the patient after we did the integration between the CEREC and the Galileos. After implant placement by the local periodontist- the patient presented back to the office for provisionalization. We figured the best way to provisionalize immediately post surgery was to bond in a single wing maryland bridge as the surgeon felt the implant was not stable enough to support an immediate restoration. The Maryland bridge was bonded wiht a single wing so as to allow the patient clensibility of the area and satisfy her esthetic needs:
Well unfortunately this case didnt last long. Soon after the initial implant placement, the implant was lost due to pain and infection. The implant was removed and the area was grafted and a new maryland bridge placed. Fast forward to today as Im getting ready for the May Live Patient Implant seminar and doing the prep work. I took a follow up photo and this is what I see and I sent to Farhad:
Its been several months yet the area is still not healed. There is irritation at the tissue and to complicate things further, the patient is pregnant so taking an xray is not an option currently.
So my question to you all is - how would you handle this in your offices? Unless this resolves in a few weeks, the patient will not be our patient for the implant seminar and I will get a new patient. But I figured this would be a good case for discussion among the group. If we dont use her in May, we can use her in the fall seminar.
Regardless, all of this will be covered in the seminar including how to fabricate the maryland bridge, how to fabricate a screw retained provisional and really every step of the implant process. But I figured it would be a great topic to stir up some discussion and talk about the potential complications of implant surgery and more importantly how to manage these complications.
Im sure Farhad will chime in here but Id love to get a vast array of opinions.
- Would you place an immediate implant after extracting #7?
- Would you be comfortable loading the implant? What is your criteria on whether to load immediately or wait?
- How would you handle the complication of having to have the implant removed? how long would you wait to place a new implant?
- If you saw the tissue that you saw in the final photo- what would your next step be?
I think we learn more from failures than from successes. Im hoping this can be one of those instances.
- Would you place an immediate implant after extracting #7? No. Having done several successful immediate placements I've also had a few fail too. Vertical fractures of roots seemed to be the common denominator. Septic sites and probably labial bone loss. For me this would now be an extraction and an acrylic flipper. Possible graft at extraction with a membrane depending on the clinical presentation and patient acceptance.
- Would you be comfortable loading the implant? No
- What is your criteria on whether to load immediately or wait? Rarely if ever load except maybe virgin bone premolar sites with solid bone and a temp way out of occlusion.
- How would you handle the complication of having to have the implant removed? Remove failed implant and again may or may not graft and I'd put the flipper back in. I know this is a young female patient and acceptance of that type of provisional is difficult but I'd insist at least till the tissue is healed.
- how long would you wait to place a new implant? 4-6mo
- If you saw the tissue that you saw in the final photo- what would your next step be? Remove the Maryland bridge and place patient in a flipper till healed. Probably a hormonal induced tissue response to gingival irritation.
- Would you place an immediate implant after extracting #7? Not an emphatic no, but most likely no. I agree with David. My criteria, being on the cautious conservative side, is any complications or infection, then TE and socket preservation graft and temporize with either flipper or Maryland (one wing of course.)
- Would you be comfortable loading the implant? What is your criteria on whether to load immediately or wait? I will most often try to avoid immediate temporization, have only done it a couple times. So am I comfortable with it, never, makes me nervous. I would like to get 35+ ncm torque on placement and into good virgin bone
- How would you handle the complication of having to have the implant removed? how long would you wait to place a new implant? After removal and grafting, wait minimum of 4 months but would like to drag it out to 6 to place 2nd implant.
- If you saw the tissue that you saw in the final photo- what would your next step be? CRY!!!!!!!! With not being able to take a film (drape the patient and take 1 PA film) I would remove the Maryland and replace with flipper, put on Peridex and Crest Pro Health w/ CPC ( i really like this stuff). Re-Eval regular basis.
I go to see this patient and talk to her about this a couple weeks ago when doing ACCEPT course. Hoping it works out for this new momma.
.
Sam,
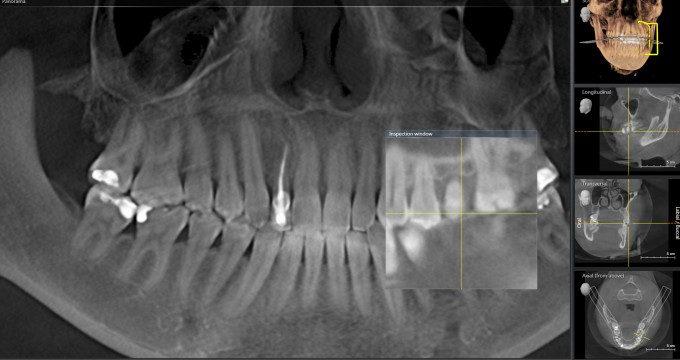
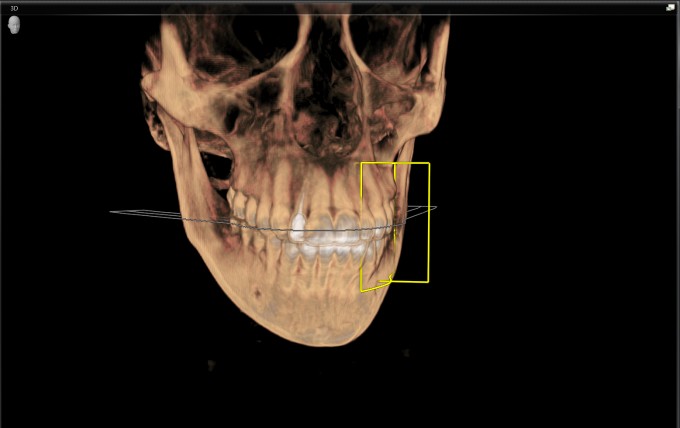
Could you post a cross section view of #7. That view would let me know how much bone buccal - lingual is present. If I can place the implant 1.5-2.0 mm palatal to the buccal plate, then I would extract and place immediately with a graft between the implant and the buccal wall. If the space is too narrow buccal/palatal then I would extract and graft. If I can get >35 ncm at insertion, then I would also place a temp to try and maintain the papillas. At this point, I agree with David with regard to the hormonal cause at the Maryland bridge site. Before I would remove it, I would re-contour the gingival area of the MD bridge to leave a space between the pontic and tissue and see how she responds.... I just hate flippers.
do u have an xray that shows the placement of the implant , the path of the tooth root appears to be not ideal for an immediate ?
The topic of immediate implant placement is very complex. I will cover this topic in detail at the Implant Seminar in May and then at the Mentor meeting in October I will cover complications from immediate implant placement. BTW: Socket grafting is not always the correct alternative treatment option.
I was not involved in the initial treatment of this patient. A local periodontist in Scottsdale (who BTW is a great clinician) placed the implant and the subsequent bone graft. At this point I would want to evaluate the pre-op CBCT cross-sectional view, the pre-op Galileos implant plan and the immediate post -op implant placement PAX. I would also want to find out what type of implant was placed and how the bone grafting was done (materials and technique used).
I agree that the current tissue reaction is due to a hormonal pregnancy gingivitis/pyogenic granulomatous reaction. In addition to the above mentioned recommendations by everybody I also recommended the application of the PerioSciences antioxidant gel.
I also recommended to postpone this patient's surgery to the Fall implant seminar, not only due to the current tissue reaction but also because she may be breastfeeding in May and although it is not a huge issue or concern it's probably just safer not to perform any elective procedures with IV sedation during that time.
Farhad
Jeremy,
You make some good points just 2 things:
1.) No need to wait 5-6 months for integration with the current implant surfaces. With the SLActive Straumann implants I could theoretically load at 3 weeks per FDA approval but I typically wait 2 months and load then (in this immediate implant placement scenario).
2.) I highly recommend against placing a larger diameter implant at the time of any implant removal, anterior or posterior but especially anterior. One miracle at a time.
Farhad
On 3/3/2016 at 4:06 pm, Daniel Butterman said...Sam,
Could you post a cross section view of #7. That view would let me know how much bone buccal - lingual is present. If I can place the implant 1.5-2.0 mm palatal to the buccal plate, then I would extract and place immediately with a graft between the implant and the buccal wall. If the space is too narrow buccal/palatal then I would extract and graft. If I can get >35 ncm at insertion, then I would also place a temp to try and maintain the papillas. At this point, I agree with David with regard to the hormonal cause at the Maryland bridge site. Before I would remove it, I would re-contour the gingival area of the MD bridge to leave a space between the pontic and tissue and see how she responds.... I just hate flippers.
Ill try to dig up the xray and post the cross section here. Ive gone in and cleaned out around the pontic area but there is nothing there- no bone spurs or cemetn or anything, just some irritated tissue.
The whole issue of immediate vs delayed is a complex one and Im glad Farhad has this on his list of things to cover at the implant seminar. Some great posts by everyone- let me get the cross section for you guys to review.
On 3/4/2016 at 10:56 am, Jeremy Heldt said...Thanks for weighing in Farhad. I think maybe there's a misunderstanding.... at 3 weeks you're loading the implant with a provisional, right? I originally meant 5-6 months for uncovering and restoring a buried implant for the final restoration.
Jeremy,
The Straumann SLActive implants are FDA approved for full functional loading with a final restoration at 3 weeks. However, this is not necessarily for an immediate implant. In that case I am comfortable to uncover and restore with a final restoration at 2 months.
Farhad
So here is my two cents worth.
1. Would you place an immediate implant after extracting #7? There are a lot of variables that go into this decision. With a root fracture it really depends on where the fracture is and how much bone loss has occurred. In the first picture it looks like the buccal tissue is looking a bit edematous. If there was any buccal bone loss due to the fracture I graft, using the sandwich technique with a-PRF, and come back in later to place the implant. Also if there is any exudate or apical pathology I will not place an immediate implant. That site gets grafted and delayed implant placement.
2. Would you be comfortable loading the implant? No. What is your criteria on whether to load immediately or wait? For immediate loading I have to have 35+ncm of insertion torque to even think about placing a temporary immediately. Minimal to no grafting and if there is grafting it can't be at the coronal aspect of the implant. Apical grafting I might temp it right away depending the extent and the patient, both from a health hx and compliance. That brings up a point that has not been mentioned for immediate placement or load and that is patient compliance. If I have the feeling that the patient won't do what I tell them as far as diet, taking medications, not smoking etc... Then I don't even look at immediate loading. This is also true for immediate placement of the implant. Basically I have a check list and if they get to many checks it goes from immediate load, down to immediate placement and then down to delay placement.
3. How would you handle the complication of having to have the implant removed? how long would you wait to place a new implant? I would remove the implant clean the site well and then sandwich graft the site to see how it looked. Then wait 6 months for the graft to mature. Then come back in and place the implant with CTG if needed.
4. If you saw the tissue that you saw in the final photo- what would your next step be? With the pregnancy as stated it may be causing a lot of the response. If that wasn't the case take a cbct to see what it looks like. Antibiotics to correct any infection and then rebuild the site with grafting. If there is still infection present upon entry then clean the area and graft.
On 3/4/2016 at 7:47 am, Farhad Boltchi (Faculty) said...Jeremy,
You make some good points just 2 things:
1.) No need to wait 5-6 months for integration with the current implant surfaces. With the SLActive Straumann implants I could theoretically load at 3 weeks per FDA approval but I typically wait 2 months and load then (in this immediate implant placement scenario).
2.) I highly recommend against placing a larger diameter implant at the time of any implant removal, anterior or posterior but especially anterior. One miracle at a time.
Farhad
Do you really feel comfortable loading SLActive that early? I'm starting with straumann and my rep had told me the same thing but would love to have real world recommendations
I usually wait 3 months just to be safe.
I'm almost to the point of never immediately provisionalizing lateral incisors. This scenario represents over 50% of my failures.
That's been my same experience in implants no mater the manufacturer...I would just rather take it slow and steady. Biology is so complicated, why risk it? My question is: if I had a hip replacement , would I start using it at the early end or late end of the recommended spectrum?