The most important part of implant planning part 2
Last week I talked about the importance of planning the implant restoration prior to doing surgery, in order to avoid complications.
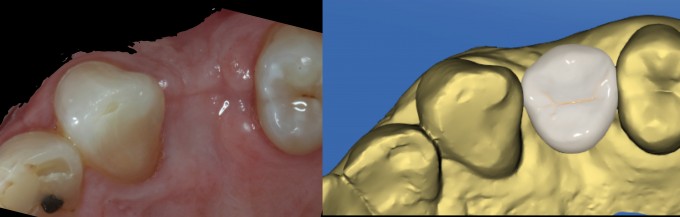
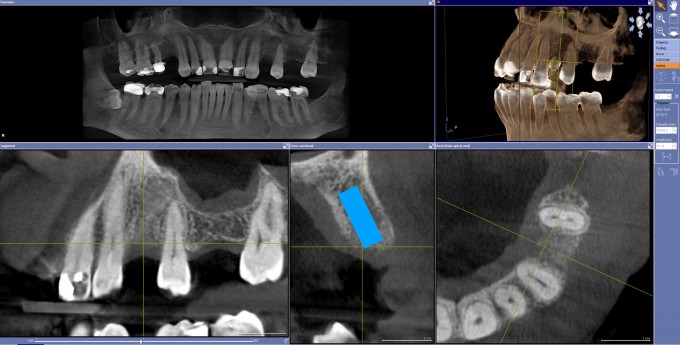
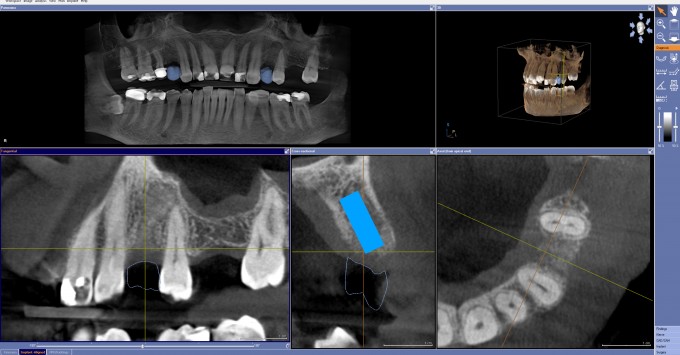
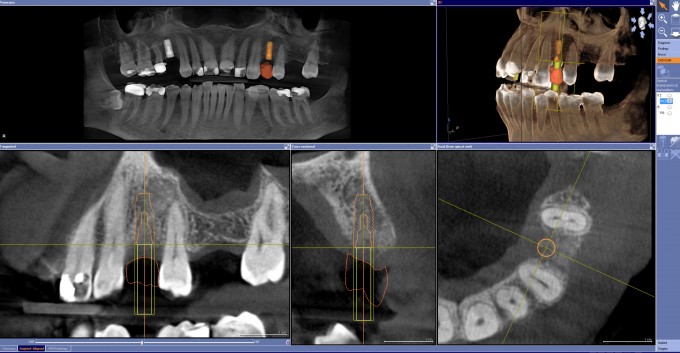
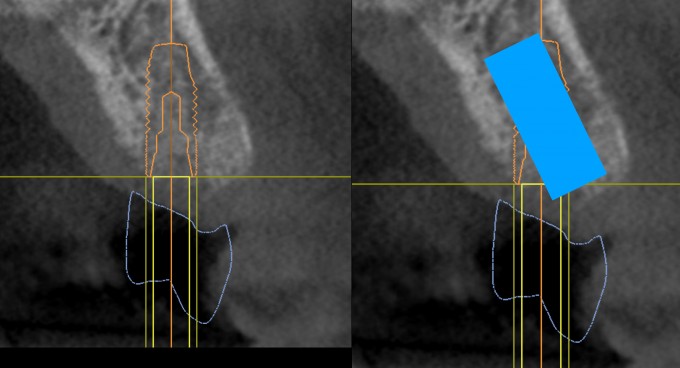
I want to take it a step further, it's equally important to export the crown design as an .SSI file and import it into Galileos Implant for planning. This patient has multiple missing teeth, and agreed to implant treatment @#12. If I would have only planned the implant in my CBCT planning software, without regard for the restoration, it would have been a restorative nightmare.
Just involved in an implant case that was placed by a periodontist that demonstrates why what you are presenting is the way to go. Tooth #9 developed peri implantitis after 4 years. IMO, and I discussed this with the patient when I restored it, the problem is the implant was in a very poor position, angled to the facial and distal toward #10, with less than 2mm between the head of the implant and the mesial aspect of the root #10. Screw down not possible and used a gold abutment and Emax crown. Looked great but not biologically compatible but took 4 years to rear it's ugly head. In discussing tx options with periodontist, he got very upset because he put the implant "where the bone was" and claims it is the restoration's fault not his. My response is/was that you have to plan from the restoration down to get the best long term result. He doesn't believe that, so what do you do? I've told the patient that long term we may have to do crown lengthening and a crown #10 to create space and if that fails, abandon the implant and do a three unit bridge. The periodontist went crazy on me. So we know that planning crown down is the best way to tx plan implants but many specialists push back on the idea. it complicates things for them, requires more grafting, etc. I am going to do all implant planning for my patients, even if they are having the implants done at the specialist, using this concept and mill or get custom guide splints and send them to the specialists so that I reduce the chance of these nightmares happening in the future.
Ross,
It sounds like you need a new specialist. Now I have a concern with your idea of planning these cases and sending to the specialist. I bet they won’t use it and many don’t have guided kits. So then what do you do?
Dan, great info and great case. I’m curious what you do in these situations when the guide sleeve impinges on the adjacent teeth. It looks like a Medium sleeve may in this situation. It happened to me a lot in premolar areas. Do you plan it at the D2 for a longer implant to move the sleeve more coronally?
Jeff
Most of the specialists I refer to are on board with me treatment planning and then I just adjust for whatever guided implant system they use. This case was from a specialist I don't refer to and my patient chose him. Fortunately i'm getting to the point where I am doing most of my own implants and only refer extremely complicated, medically compromised, etc. patients to the specialists. Taking ICB in July to improve on the whole restorative/implant treatment planning and how to make it work. Lots to think about and manage but this is why I love Cerecdocs and these discussion boards. The flow of information is fantastic, thanks!
Ross - these restorative driven cases like this really does removes headaches. Once in a while back in the day I would have to try and restore those facially angled implants resulting in very poor emergence profiles and facial recession. This is what drove me a while back to dive into my own placements / planning with the crown down approach and investing in the technology. Great case to show and thank you for sharing the two scenarios.
If the neighboring tooth is closer than the biological width there will be inflammation, agree. Even for implants with conical connection.
But what do you say is the mechanism behind inflammation in the case of an angulated abutment? And wouod you apply it for any kind of implant?
Seems to me it almost always is over contouring and violating the biologic width. Both lead to problems with maintenance and eventually the inflammation causes bone loss on the head of the implant.
For the case of a conical connection I do not quite see the connection to overcontour8ng and violation of the biological width.
Would you mind explaining your points with a little more details?
(And if that is fundamentally true: Because the tiBase abutments are usually a lot more contoured than the stock or Atlantis abutments would that not mean that we should not use tiBases at all?)
Armin,
I agree with Ross here.
A conical connection and platform switching are great in maintaining crestal bone levels. However, subgingivally and especially subcrestally overcontoured restorations or restorative components essentially create a reverse platform switch effect and biological width impingement thereby negating the positive effects of the conical connection and platform switch. In addition, these overcontoured restorations/restorative components put adverse pressure on the bone and soft tissues leading to bone and tissue loss. As far as biologic width the ideal is to move the restorative interface as far away from the bone and tissue as possible while still supporting the soft tissue emergence and esthetic profile (analogous to why supragingival crown margins are always biologically more sound than subgingival crown margins).
Any tibase that is significantly wider than the implant platform is imo contraindicated and I stopped using the standard tibases for narrow implants several years ago. Nowadays I use the standard tibases (even for regular sized implants) less and less and I am more frequently using tibases with higher gingival heights or custom bases a la Atlantis. The ideal contour is a narrow subgingival contour that stays away from the bone and allows for more soft tissue volume while becoming wider in the immediate subgingival area to support the tissue emergence profile without creating a plaque-trapping concavity.
As a side note: Dan's case above shows one of the reasons why I am not a big fan of ridge expansion (with Densah burs or any other method). You can only expand the ridge in the trajectory of the ridge and that trajectory may not be the correct restorative trajectory as Dan so eloquently demonstrated.
Farhad
Farhad,
so you say if the angulation is high enough (supragigivally at best) it does not have such a negative effect?
And even more specific: Can a thin titanium abutment that is angulated already subgingivally be as tissue- and bone-friendly as the thicker, straight tiBase abutment (ceramics structure)?
I was referring rather to the ceramics structure of the tiBase-abutment-complex. It is usually wider than a stock or Atlantis abutment. I have learnt that the ideal abutment should be perfectly concave subgingivally and also perfectly smooth (without any gaps). So the tiBase is probably a compromise.
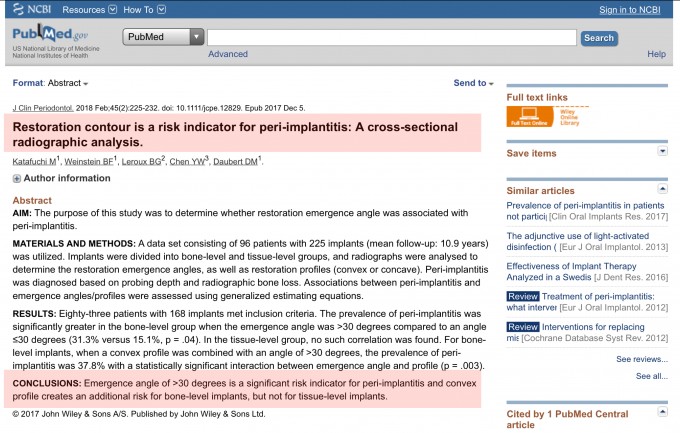
I Think a Sirona TiBase restoration can be a perfect choice in a lot of situations, you just need to choose the right indications for it. There is interesting research regarding over contoured, convex abutments that may lead to peri-implantitis in bone level implants. I think keeping the abutment as concave as possible and moving the restorative platform away form the implant platform in bone level implants is the safest way to treat.
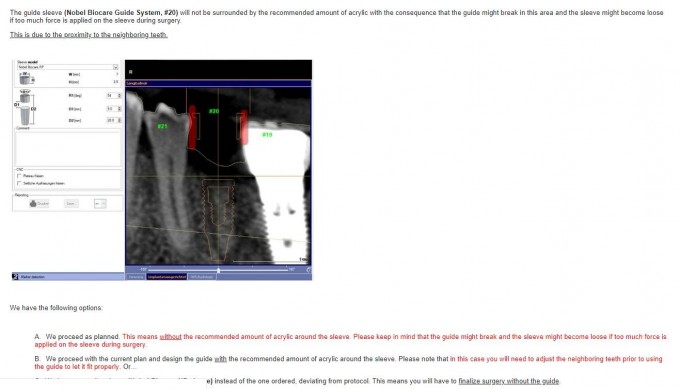
On 5/18/2019 at 8:25 am, Jeffrey Gregson said... Ross, It sounds like you need a new specialist. Now I have a concern with your idea of planning these cases and sending to the specialist. I bet they won’t use it and many don’t have guided kits. So then what do you do? Dan, great info and great case. I’m curious what you do in these situations when the guide sleeve impinges on the adjacent teeth. It looks like a Medium sleeve may in this situation. It happened to me a lot in premolar areas. Do you plan it at the D2 for a longer implant to move the sleeve more coronally? Jeff
Ross, I'm not sure that sending a surgical guide to the specialist and insisting that he use it is the way to go. This is more about sharing information so that everyone gets a heads up prior to surgery. If the patient understands what the restoration will look like and the surgeon understands where the implant should go in relation to the restoration with a quick and easy picture, that alone will save many headaches.
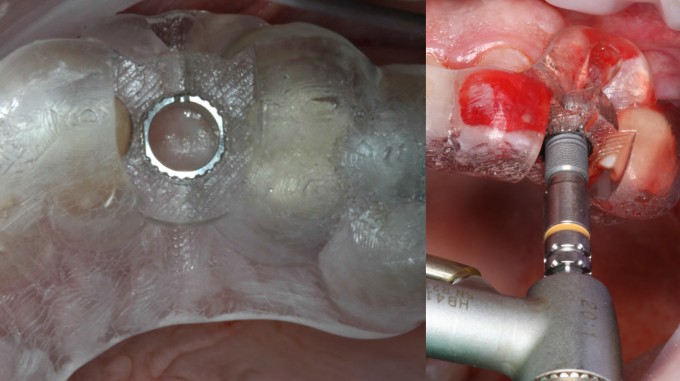
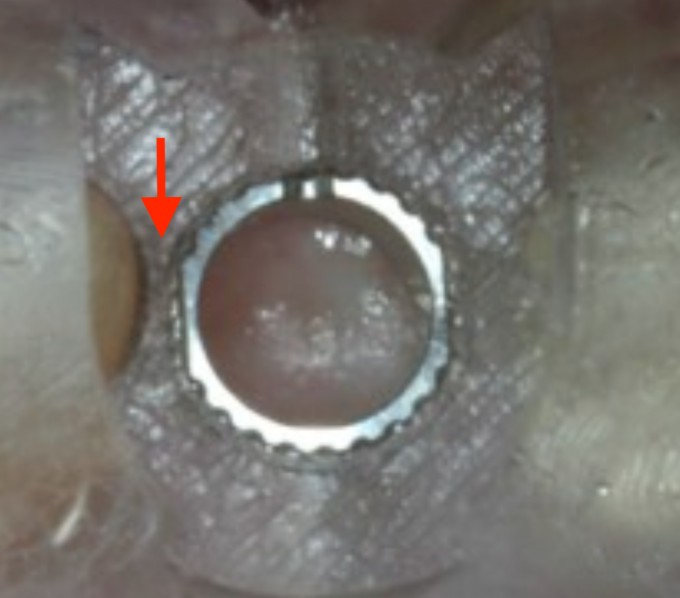
Jeff, good eye. A lot of times you can get away with a tight space by using the "grind out" feature around the guide hole during the cg2 design. Adjusting the D2 to raise the guide platform can also work, but that can cause errors with incorrect calculations and the patient will need to open very wide to accommodate the guide. This case was pretty tight for sure and I find that a simplant guide made with Azento can fit in many places where a cg2 might not be able to. Here is a photo of this guide and implant placement:
On 5/19/2019 at 6:22 am, Daniel Butterman said...I Think a Sirona TiBase restoration can be a perfect choice in a lot of situations, you just need to choose the right indications for it. There is interesting research regarding over contoured, convex abutments that may lead to peri-implantitis in bone level implants. I think keeping the abutment as concave as possible and moving the restorative platform away form the implant platform in bone level implants is the safest way to treat.
Tx, Daniel. This critical information is new for me. Can only find the abstract and not the full article.
My question would be if the study differentiates platform-matching and platform-switching implants.
I have used quite a few 38° Stock abutments with conical connections so far. All of them are still in function. But I am open to re-evaluate this strategy.
The angulation is happening above tissue level in those abutments. Maybe comparable to tissue-level implants? This would relativize the negative effects maybe.
If anybody has deeper information about this I would like to get to read it.
Armin,
If the abutment/restoration angulation is supragingival then it has no negative effects. In esthetic areas the subgingival angulation can also lead to facial recession of the gingival margin leading to an unesthetic outcome in addition to the aforementioned problems. That's the reason that I recomend to never plan the implant position such that the implant is emerging past the incisal edge.
Farhad
Tx, Farhad. Any (online) literature that you would recommend?
And another important question for me: are angulated Atlantis abutments angulated subgingivally or like my stock abutments supragingivally?
Dan,
I recently had a case with 12 and 13. Tight fit and I wasn’t able to do fit both sleeves. I could only do 2 3.6mm implants due to the space between the implants. With that I had 2.8mm between.
With that said, I used Cadray and had a guide printed with no metal sleeve but rather the printed resin was the diameter of the Astra sleeve and the D2 calculated. Do I have other options in these types of cases besides cadray? Cg2 was not a great option here. And she had a mouth full of pfms so there was a lot of scatter. I have t placed them yet. Planning to in August as she just had a joint replacement.
Thanks
On 5/19/2019 at 9:54 am, Jeffrey Gregson said... Dan, I recently had a case with 12 and 13. Tight fit and I wasn’t able to do fit both sleeves. I could only do 2 3.6mm implants due to the space between the implants. With that I had 2.8mm between. With that said, I used Cadray and had a guide printed with no metal sleeve but rather the printed resin was the diameter of the Astra sleeve and the D2 calculated. Do I have other options in these types of cases besides cadray? Cg2 was not a great option here. And she had a mouth full of pfms so there was a lot of scatter. I have t placed them yet. Planning to in August as she just had a joint replacement. Thanks
I don't love the idea of running the EV drills at high rpm against a resin guide without a metal sleeve. If you can't make a cg2 work, you could try a Sicat guide, but I'm not sure if that will be much better in a tight space. If you don't want to do a full Azento case, you can just order a Simplant guide, the sleeve is very thin and the amount of resin to support it is much less than a cg2.
What’s the difference between a Simplant/Azento Guide and a SiCat Guide? Are the EV sleeves with a Simplant Guide any different than the sleeves with a SiCat Guide?
Farhad
On 5/19/2019 at 8:56 pm, Farhad Boltchi said... What’s the difference between a Simplant/Azento Guide and a SiCat Guide? Are the EV sleeves with a Simplant Guide any different than the sleeves with a SiCat Guide? Farhad
I have a request into DSI to find out the outer dimensions of the Simplant EV sleeve and will post it here when I have it, but maybe someone can get the dimension of the Sicat sleeve?
What would be very helpful to find out is the minimum required space between 2 teeth in order to manufacture a Sicat, Simplant, and future cg3, all with an Astra EV ND sleeve. This way, a choice can be made between guides when there are very narrow spaces to determine if just a pilot hole will be guided, or full implant placement.
Agreed dan. The only good thing would be the sleeve would be against the resin not the drill.
Interested in the other info as far as space and sleeve sizes. I will certainly look into simplant. What do I have to send to simplant for a guide? Do they accept io flo also?
SiCat uses the Steco sleeves for their Astra EV guides, which can be ordered through SiCat or Steco (Aeton Medical here in the U.S.). The dimensions are as follows:
WD: Inner diameter=5.2mm.....Outer diameter=6.0mm
ND: Inner diameter=4.6mm.....Outer diameter-5.6mm
I do not know what sleeves Simplant uses for the EV but I can not imagine that the dimensions will be much different due to the need for the tolerances involved. In my opinion the mesio-distal dimensions for a SiCat guide, a Simplant guide, and a CG3 will be very similar.
For CG2: If there is mesio-distal sleeve impingement it can be "ground out" by the software. That software function only applies to apical impingement of the sleeve on the tissue. I think the software will not even allow one to move forward if there is mesio-distal sleeve impingement.
Alternative: For tight spaces a lot of times I choose the SiCat sleeve-in-sleeve system. For the Straumann system that still allows me to use the 3 first drills fully guided so that I can place up to 4.1mm implants. The crestal profile drill and the implant placement are non-guided in that case. This has helped me in many tight spaces.
Farhad
Farhad,
Can you explain the sleeve in sleeve more? I have seen the option but never used it. I’d like to know if it’s an option for me in future cases right on space with Astra EV. I just understand more when I see it.
Thanks,
Jeff
The sleeve in sleeve is just like it sounds. There are removable sleeves that fit in the fixed sleeve in guide, kind of like the key idea without handles, etc. I think they will only provide 2-3 sizes depending on what implant you are using, but Farhad can maybe give better info on that. What I don't like is they come out on the drill when using pumping motion sometimes. Otherwise, I used a lot before using Digital guides as I rarely prepare the whole site guided anyway.
Like Farhad, I use the sleeve in sleeve when the implant would be tight (lower anterior), or the sleeve/sleeve housing would be impinged upon by the adjacent teeth.
You can pick your sizes. For Straumann, I pick the 2.2/2.8 sleeve in sleeve, and for Nobel I use the 2.0/2.8. These sizes correspond to the first two drills in the system.
If you're using a 3.3 Straumann, you're done after the 2.8 anyway.
If you're using the 3.5 Nobel, I do the 2.8 Active drill for active, then place the implant, or for the conical, I do the 1828 Densah through the 2.8 sleeve, then the 2535 through the opening with no additional sleeve. I then have to place the implant without the guide.
The third choice got blocked out in the snip, but that's the sleeve in sleeve choice, which is what I told them to do.