Is it possible.....
.....to place an implant and graft simultaneously and achieve an acceptable outcome in this case?
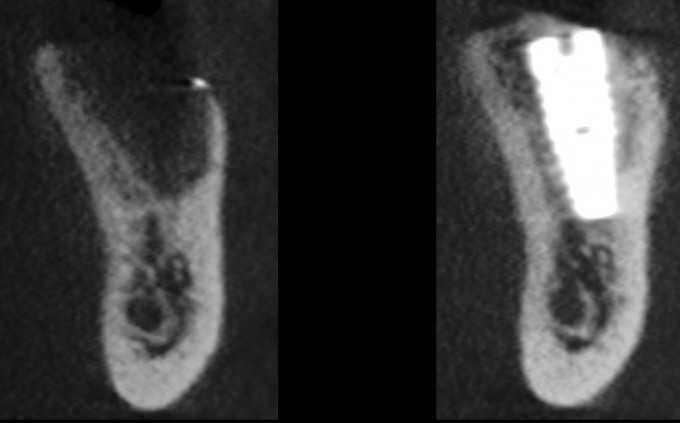
Let me give you some background: the patient is a 74 yo male, medical history includes type 2 diabetes and hypertension, for which he takes meds and both conditions are controlled. He had #19 extracted at another office approximately 8 months prior to the CBCT images you see above. He has adequate thick attached tissue and restorative space. He has had a couple of other opinions provided already.
His ask is this: he wants an implant placed and any defects grafted in one procedure. He is aware that he will have to return at some point later on for the crown, he just does not want to have multiple surgeries if at all possible. He desires this because he's not getting any younger and doesn't want to spend any more time than he has to away from his job and his vacation house.
What do you think? Tell him he has no choice but to perform a ridge augmentation first? Go for it with the understanding that there may be complications that require more surgeries to correct?
Good question. I'm doing one just like it on Monday. With your skills Jeremy, should be no problem. Risk of failure is higher.
Appreciate the vote of confidence, Eric!
In your opinion, what are the biggest obstacles to success here? What might I need to pay special attention to? Is there a preferred graft material or membrane type here? Let’s see if we can inspire the group to work on a thought process together
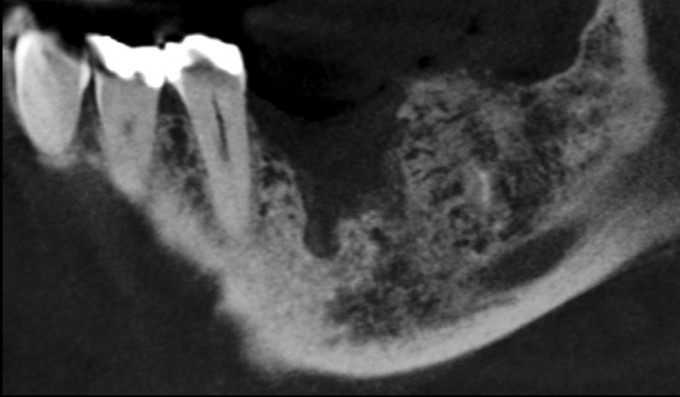
the only question is how are you going to get primary stability for the implant, grafting this doesnt seem to be the obstacle as you have tons of wall
Excellent point; lingual wall is intact, leaving the grafting mainly to the buccal with a little medial and distal. We’ve only got a few millimeters above the nerve here. So that bone and the lingual are all that’s available for stability.
On 11/9/2017 at 4:28 pm, Jeremy Bewley said... Excellent point; lingual wall is intact, leaving the grafting mainly to the buccal with a little medial and distal. We’ve only got a few millimeters above the nerve here. So that bone and the lingual are all that’s available for stability.
jeremy i will be happy to refer these to you all day just send the restorative back to me when your done, i am sure you planning to relocate the nerve here and use the canal for primary stability. hah
I️ would want to know the genesis behind his tooth loss. Judging from the X-ray, I️ would assume that it was some sort of infection. It’s true that implants will never get an endodontic infection, however the biology that supports and sustains an implant is still susceptible to periodontal pathogens. When a patient doesn’t truly understand these risks are associated with an implant just as they are with a tooth, they begin to look at implant therapy as a simple end all procedure. This simple way of thinking makes them ask things of us that are “possible” but not always in their best interest. I️ think to do what the patient is asking is possible but not highly predictable. The extraction site, I’m guessing from the X-rays, had all five walls present post TE. From that assumption, I️ would expect to see a little more healing at 8 months even without a graft. It makes me question how well the socket was cleaned out after TE and how large the infection was that led to the tooth loss.
That would be highly unpredictable. Variables like final crestal position, blood supply, and osseointegration are hard to predict in this case. I personally would do three stages here.
There is definitely literature out there to support simultaneously implant placement and bone grafting. From what I have read, the literature shows promising results for this with small to medium sized vertical wall defects (<5mm).
Though there isn't much bone present currently, the buccal wall is thin and short, but the defect compared to the lingual appears to be less than 5mm. If you can achieve primary stability of the implant, I think grafting in conjunction with the implant placement is doable. I'm not well versed enough in the type of membranes or bone grafts that you specifically may choose for a case like this. Knowing Jeremy, I think PRF, Mineross, and Cytoplast d-PTFE membrane are involved and burying it for 4 months +.
Without much native bone to engage, are others thinking that they will utilize an implant with a more aggressive threading and pitch to help get more primary stability?
Bump...being a newbie to implants I would personally love to hear thoughts on this case. And if you were to attempt this, how would you go about it specifically
Based on the information provided thus far everyone is just guessing right now. Let's see where the final restoration is going to be and where the implant position is going to be according to the desired restorative outcome...Then we can start having a better discussion regarding predictability, etc.
Farhad
JB. Looking at the image I WP of like to see some better density in the socket 8 months post extraction. In my office I don’t think I am comfortable doing everything in 1 visit. By the time you scoop the mash potato bone out there will not be enough wood to hold the screw IMHO
I had a similar case recently where I was planning to extract, place, and graft. I decided to punt during the procedure when I could not get the stability I wanted. I ended up grafting with 50/50 MinerOss followed by PTFE membrane and sutures.
There are a lot of things we “can” do but the question is if it is the best tx plan. If implant stability cannot be achieved then it becomes a graft and implant later procedure IMO.
In regards to materials, we would want a bone graft material that has traditional turnover time. We want de novo bone to either quickly attach to our implant or prepare the socket to receive an implant in a few months. This is considering the area of the mouth and a fairly intact buccal plate.
Unless a large flap elevation will be used then we will need a non-resorbable membrane to isolate the graft and prevent tissue creep. I have been a PTFE fan for a long time.
This is a great discussion as this is a situation we all may encounter frequently.
Okay let's keep this moving along.
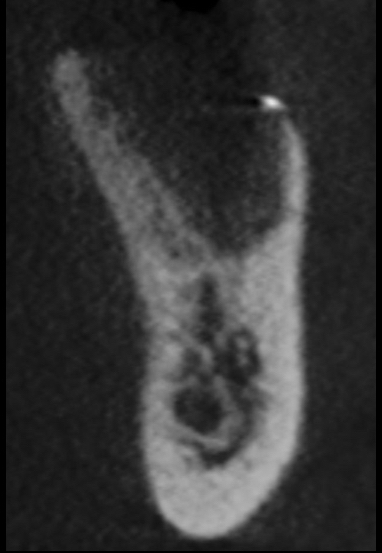
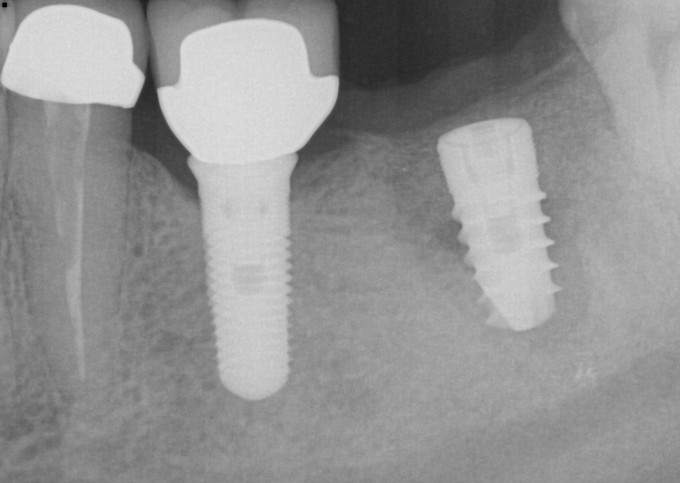
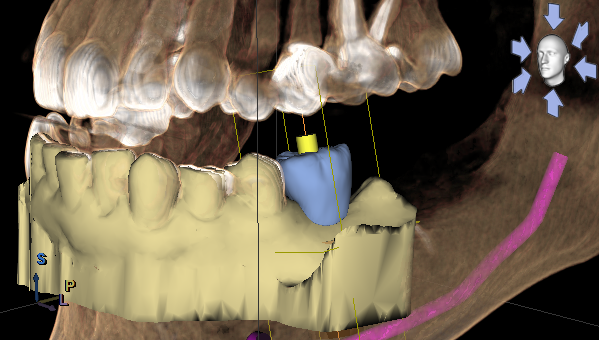
Excellent points made by everybody, largely centered around ways of surgically treating the case, and these are very important aspects of treating this case. One thing Farhad said really stood out to me, and makes me ask the question: why are we placing the implant? What's the point of it? The answer, of course, is that the point of placing an implant is what is supposed to go on it at the end of treatment. This thought process is beautifully demonstrated in a practical way in the integration of Omnicam and Orthphos SL CBCT. So here's the initial proposal and plan I worked up, the goals being to choose a fixture of adequate size for the clinical situation, to achieve primary stability, and of course it needs to be in the prosthetically correct position. Once those are established, in my mind anyway, we can start thinking about the feasibility of grafting around this proposed fixture site:
What are your thoughts on this proposed implant size (5.8mm diameter) and planned position, seeing the proposed prosthesis and knowing that the goal is to graft around the implant at time of placement?
Jeremy
Sometimes you will be surprised in that low density bone on the CBCT scan after extractions is still good viable bone to receive an implant.
The position of the implant looks good. I think Matt pretty much nailed it in all his statements above. Plan the case, fabricate a guide, flap the case and see if your implant can achieve primary stability. If so, place the implant and do a layered buccal bone augmentation grafting...otherwise re-graft and stage the case.
Farhad
Thanks Farhad
I find that there’s always at least a little more bone than what we see on the cbct, and that the barely visible low density stuff is indeed usually useful. There’s a radiological term for this that’s escaping me at the moment, but it has to do with limitations in cbct technology.
Yes it is very possible.
8 months of healing is excellent
A one visit implant placement and contour augmentation with 50% Bio-Oss ( non resorbable ) and 50% Autogenous bone locally harvested.
Place the 1.5 mm cover screw or 2 mm and build the bone to it. Cover the implants with Bio-Guide, Release Flap and completely bury implants.
Do not forget to perforate the cortical bone buccaly.
A note: in order for the bone graft particles not to slide down from the graft site ( Gravity ), you need to flatten the cortical bone buccally, I.e create a balcony or place 2 pins into the Bio-Guide then fill the area with the 50/50 graft
There is sufficient bone and the IAN is low, CBCT's all the time shows bone like that.
Open a large flap
Collect Autogenous bone, Mix with Bio-Oss 50:50 or any combination is better than no autogenous in the graft
Place implants Guided or free hand
A longer and thinner implant is better
e.g a 4.1 Roxolid Straumann Tissue level or 2 NNC Roxolid 3.5 mm tissue level( in #19 &18 ) I prefer 2 implans splinted. Pt has a max 2nd molar.
Primary stability should your be your least worries.
Good luck
Faisal
Farhad you nailed it, as always. Be prepared for best case scenario: open it up, evaluate the site, and have a guide ready. I've had a few cases that looked like they would be a good outcome and after prepping the osteotomy found I had 0 stability with the implant. Luckily I was willing to back it out, graft, close up, and re-access in 4-5 months. Its a bummer, but it happens. Other cases that looked more questionable give great initial stability for the implant and concomitant grafting gave a great solution.
Good surgical plan JB, I think you'll nail this one.
Great great discussion everyone, thank you for the input! So in general, the opinions seem to be that the most important aspects of a case like this are:
1. Primary stability
2. Graft containment
3. Primary closure
I completely agree with all of these opinions. I was expecting there to be a little more discussion about what types of membranes were most appropriate, and whether or not it was even appropriate to attempt this in a single stage, but on reflection it occurred to me that our community here is far more advanced than your average group of clinicians, so it really shouldn't surprise anyone that most felt the case could be treated as the patient desired.
I actually treated this case several years ago, and have been following it over time. I find myself asking what I did well and what I could have improved, and in hindsight should I have made different choices to improve the outcome?
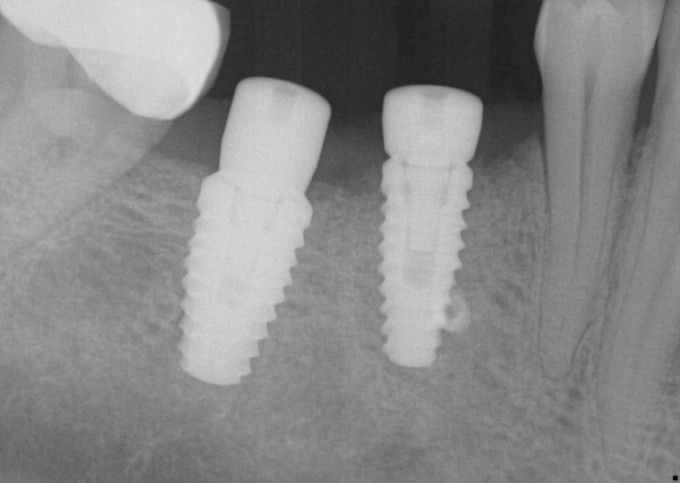
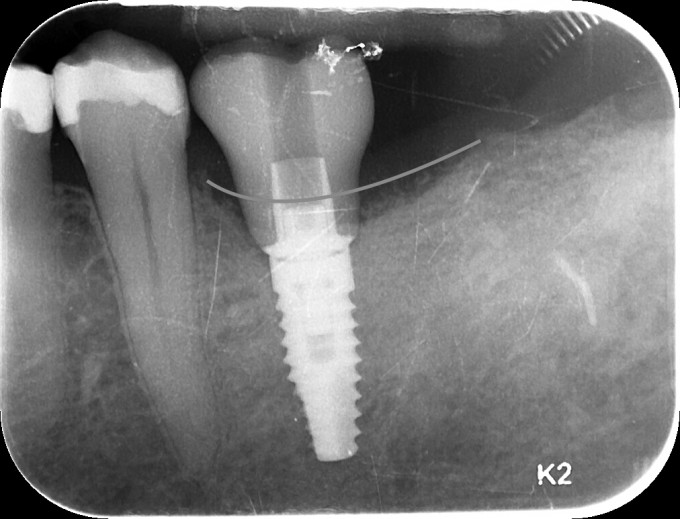
I ended up changing my plan and did not place a 5.8mm implant, opting for a 4.6 instead. I did this because I felt like I was in danger of over prepping the available bone and compromising two things, the first being primary and secondary stability, the second being losing available bone to help support the graft and its consolidation. The implant achieved excellent primary stability, approximately 40 Ncm of torque was required to deliver it to depth. I used Mineross cortical/cancellous blend and a long lasting collagen membrane that was not reinforced with titanium. I did place PRF into this graft, and also layered PRF membranes over the collagen membrane prior to primary closure. Here's how the patient returned to me after approximately 6 months of healing:
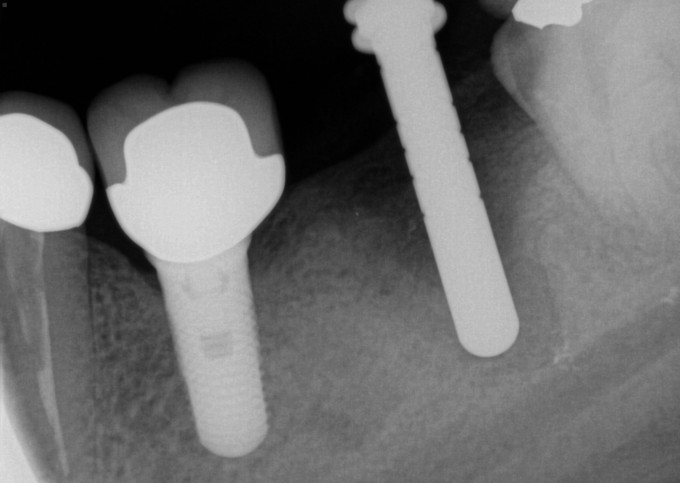
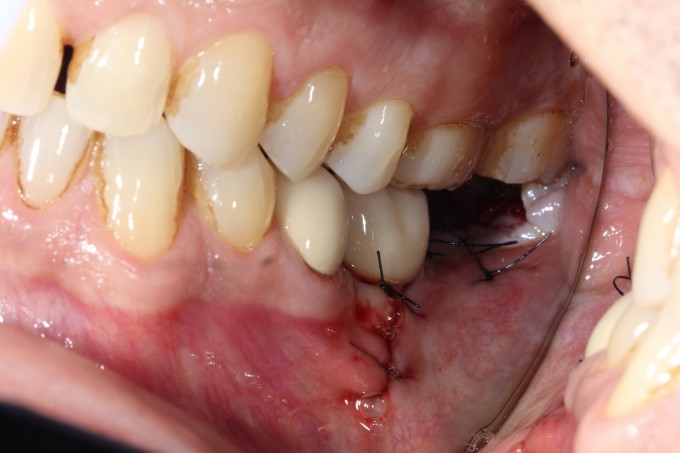
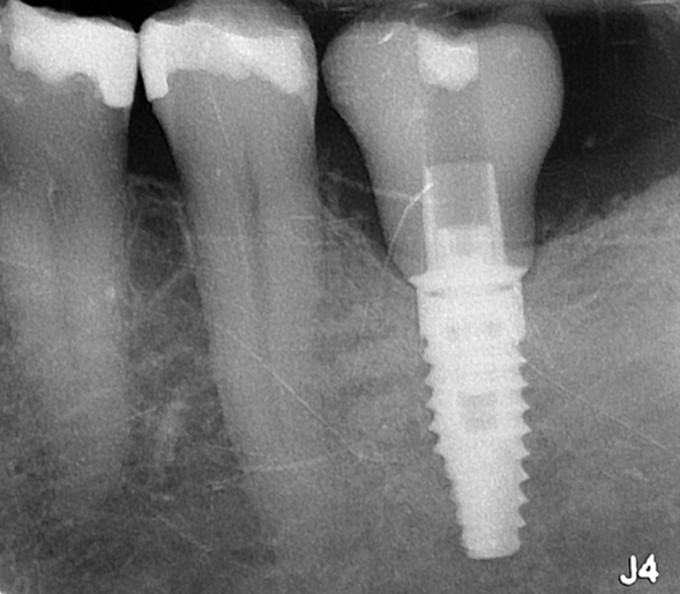
Second stage surgery involved drilling and chiseling bone off of the cover screw, and a lot of bone profiling to get the healing abutment to seat. This was thick, mature, dense bone that was not easy to remove. I restored this with a Sirona tibase and emax, and it was one of the first restorations I did with this implant restorative workflow after it was launched. Here it is at a 2 year recall:
Seeing all this info now and looking back, how should I have approached the case differently? What could I have done differently in both the surgical and prosthetic phases to improve the outcome? It's been a couple of years since that last PA; what do you predict the graft, the implant, the soft tissue, and the restoration look like now?
Jeremy
Wow...impressive Jeremy! How did the mesial bone respond to the tight emergence profile from the implant crown? Any changes there?
JB, the success you've had with this case thus far is not surprising; you're a good surgeon...almost as good as your wife. ;)
"What could I have done differently in both the surgical and prosthetic phases to IMPROVE THE OUTCOME?"
-I think you did a great job; your 2 yr recall radiograph demonstrates that quite well. This case is a 'success.' What better outcome can we ask for than surgical success and a happy pt (I'm assuming)? So if our definition of success is implant retention, minimal bone loss, ability to use restoration, etc. than you achieved that goal 100%. I believe anyone here would love to have this outcome in our office.
What could I have done differently in both the surgical and prosthetic phases to improve the outcome?
No one can argue with a beautiful outcome, especially with a multi-year follow-up...But since you were gullible enough to ask:
1.) Surgical: Use a 2mm healing cap instead of a cover screw. These were probably not available at the time you did this case but with the 2mm healing cap you could have still submerged the implant but would have had a much easier time uncovering the implant.
2.) Restorative: The follow-up radiograph looks good but the tibase restorative interface is a little too close to the bone for my taste. That's why we need tibases with varying gingival heights.
Farhad
On 12/9/2017 at 9:23 am, Farhad Boltchi said...What could I have done differently in both the surgical and prosthetic phases to improve the outcome?
No one can argue with a beautiful outcome, especially with a multi-year follow-up...But since you were gullible enough to ask:
1.) Surgical: Use a 2mm healing cap instead of a cover screw. These were probably not available at the time you did this case but with the 2mm healing cap you could have still submerged the implant but would have had a much easier time uncovering the implant.
2.) Restorative: The follow-up radiograph looks good but the tibase restorative interface is a little too close to the bone for my taste. That's why we need tibases with varying gingival heights.
Farhad
One of the reasons I find myself keeping Conelog implants on my shelf.
So to clarify your actual layering procedure in this case.
1) 4.6 Implant placed
2) Mineross bone graft.
3) Long lasting collagen membrane (What specific type?)
4) PRF
5) Another collagen membrane (What type?)
6) PRF over the top again
7) Suture closed
Am I missing anything?
Curious if others would do anything different...Farhad?
On 12/9/2017 at 11:28 am, Daniel Wilson said... So to clarify your actual layering procedure in this case. 1) 4.6 Implant placed 2) Mineross bone graft. 3) Long lasting collagen membrane (What specific type?) 4) PRF 5) Another collagen membrane (What type?) 6) PRF over the top again 7) Suture closed Am I missing anything? Curious if others would do anything different...Farhad?
I think that had I staged the case, I could have achieved more height of bone (likely to the point drawn on the above radiograph) had I used a different membrane. If I were successful in doing so, I would have had a more normal clinical crown to create later on, as opposed to the compromised tall crown I made for this patient. A couple if questions come to mind:
Should I have done it this way instead, seeing the end result?
Could I have placed a longer implant with the platform more in an ideal position and tried to graft up to that?
Jeremy
I think it turned out well in the end, but looking back I would graft and place after healing. Hard to say if you would have actually obtained the height you outlined but if you would have it would be a better outcome. The grafting you did turned out well in terms of gaining bone where you hoped to. I have no idea if you would have been able to place the implant 2-3mm higher though and gain the additional space. My other thought is how much time is really saved for the patient? If you are waiting over six months that isn't much faster then grafting in the lower mandible and re entering to place biohorizons ( recommended 10 week wait to restore). It does reduce appointments and chair time but increases stress.
Good case and thanks for posting it. It really helps watching and learning from people who push it a little bit and are willing to share their results. Also good documentation and plan.
Dave
Great case JB. I think too often in dentistry we don’t look back and analyze/reassess our cases from the past, especially when they are successful. As this case shows, think there is just as much to learn from successes as there is from failures. Especially when you have such good input from other experienced/knowing minds. Thanks for sharing.
On 12/11/2017 at 8:13 pm, Jeremy Bewley said...
I think that had I staged the case, I could have achieved more height of bone (likely to the point drawn on the above radiograph) had I used a different membrane. If I were successful in doing so, I would have had a more normal clinical crown to create later on, as opposed to the compromised tall crown I made for this patient. A couple if questions come to mind:
Should I have done it this way instead, seeing the end result?
Could I have placed a longer implant with the platform more in an ideal position and tried to graft up to that?
Jeremy
I doubt that you could have achieved (and maintained) that bone level with a staged approach.
The clinical crown length has never shown to be an issue in implant dentistry. I think the tibase restorative interface and the reverse platform switch is more of an issue in this case than the length of the crown.
Farhad
Thanks for the replies everyone, and for drilling down with me on the details
I think with the height of bone available on either side of the implant (mesial and distal in the PA above) I could have gained a couple of millimeters using old school tenting screws and then some sort of reinforced membrane had I staged this case. Of course I would agree that it is less predictable than the bone I gained in this case, but I think possible.
Farhad, isn't it that a high crown:root ratio in implants hasn't been shown to be problematic? My issue with situations like this isn't the actual ratio, but in deep soft tissue recesses that make maintenance a challenge. In other words, chronic food impaction with difficulty cleaning, leading to peri implant mucositis, leading eventually to peri implantitis. A more regular relationship of prosthesis to tissue minimizes this particular challenge.
It's important to remember that probing depths in implants don't mean the same thing as they do around teeth. Teeth average about 2.04mm probing depths in health, but normal may be greater than 4mm in some sites. Implants average 3.3mm but this can vary wildly from site to site; a perio probe reading around an implant may simply reflect the preoperative thickness of soft tissue, and have nothing to do with the health of the peri implant tissues. Sulcus depths 5mm or greater are unlikely to be cleaned adequately, and this can increase the chances of chronic inflammatory problems around the fixture. Some more context for this point:
In teeth there is a connective tissue attachment that resists a probe from penetrating to bone; this attachment is a true mechanical barrier that acts as a biologic seal and resists advancement of bacteria. In teeth there are 11 gingival fiber groups, and at least 6 of these insert into cementum.
There are only 2 CT fiber groups around implants, and neither attaches to the implant. There are hemidesmosomes from the junctional epithelium that act as a biologic seal, however the collagenous parts of the linear body of the attachment cannot adhere to or become embedded in the implant body. This junctional epithelium seal resists tearing of the soft tissue as it circles the abutment, but there is very little resistance to penetration of a probe or apical migration of bacterial plaque biofilm. This is a much more friable and delicate condition than is found around teeth.
In any case, here's a recent PA and clinical photos, approaching 4 years now. In this case the patient reports no food impaction, no difficulty cleaning the prosthesis, and somehow there is very little change of the bone near the tibase. I do not like my crown design or my stain and glaze job, however they've not contributed anything negative to the outcome of the case and only offend my sensibilities.
Jeremy