This is why i place my own implants
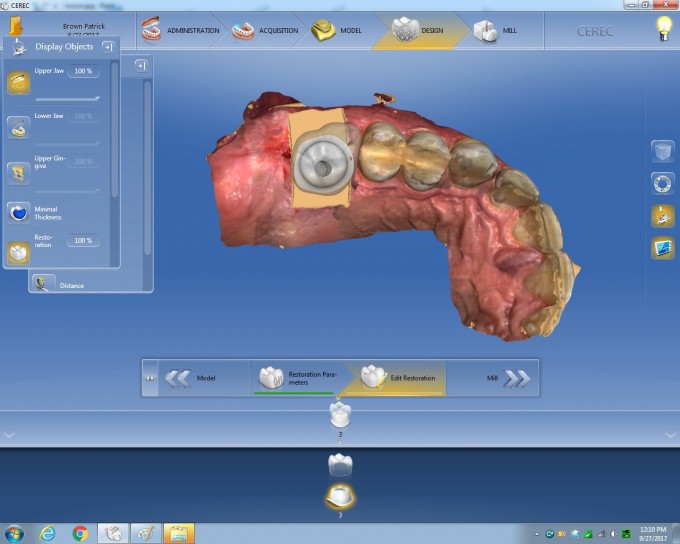
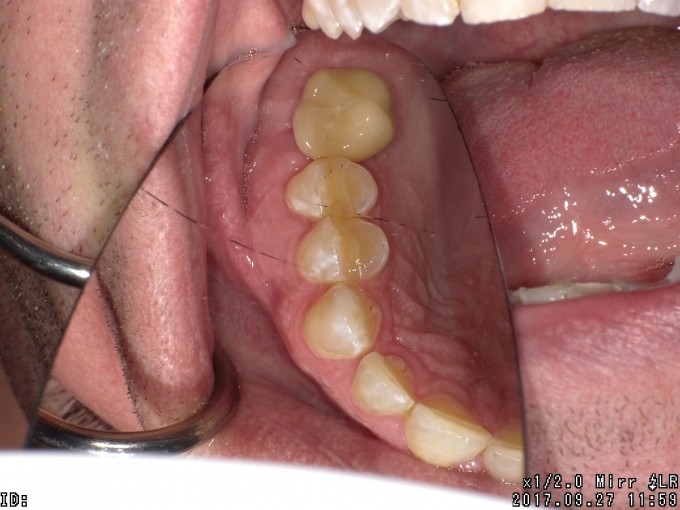
Got a new patient and he said he was ready for his implant crown. The implant was placed a out a year ago. it is so challenging to restore poorly placed implants and tales so much more time to get compromised results when there is poor planning.
the implant was too distal and too palatal. That made it more work then this should be. Just a tough case and the position compromised the final result.
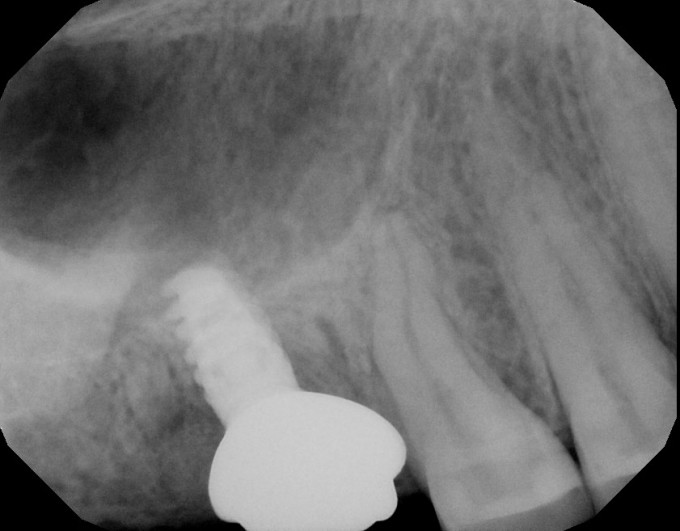
Nicely done! Did you by any chance try to probe around the implant? The x-ray looks suspicious to me. Add to that the deep placement, yet the cover screw is exposed and the purplish looking tissue around the implant and I am wondering if there is already 50% bone loss on this fixture. The DB root (and maybe a smidge of the MB) still appear to be in the bone with grafting material placed on top. I may be wrong!!
On 9/29/2017 at 12:49 pm, David Sullivan said...Nicely done! Did you by any chance try to probe around the implant? The x-ray looks suspicious to me. Add to that the deep placement, yet the cover screw is exposed and the purplish looking tissue around the implant and I am wondering if there is already 50% bone loss on this fixture. The DB root (and maybe a smidge of the MB) still appear to be in the bone with grafting material placed on top. I may be wrong!!
I was wondering the same thing....
Unfortunately, this is a far too common occurence..... The dentist/specialist places the implant and then the GP has the headache of restoring it. There are quite a few surgical specialists that need to realize that the standard of care is now restoratively driven and no longer surgically driven implant dentistry.
Winnie
Agree with above.
Any idea if the operator placed it as an immediate and just used the palatal socket ( thereby explaining the less than ideal positioning? )
Is that bleeding in the screw access?
If the patient was told by someone that his fixture was "ready for restoration" and then it fails subsequent to having been loaded by your restoration through no fault of yours or your beautifully performed restoration .... oh, boy... Hope not!
David and Leon
Exactly, I spoke to the patient and have major concerns. Did not probe, but still wondered if it would unscrew. I really leaned on it and was surprised it was solid, still informed the patient of my concerns.
I am at a quandary at times as I am just a country dentist and find it hard to send people back to the specialist.....
On 9/29/2017 at 1:26 pm, Askold Wynnykiw said...On 9/29/2017 at 12:49 pm, David Sullivan said...Nicely done! Did you by any chance try to probe around the implant? The x-ray looks suspicious to me. Add to that the deep placement, yet the cover screw is exposed and the purplish looking tissue around the implant and I am wondering if there is already 50% bone loss on this fixture. The DB root (and maybe a smidge of the MB) still appear to be in the bone with grafting material placed on top. I may be wrong!!
I was wondering the same thing....
Unfortunately, this is a far too common occurence..... The dentist/specialist places the implant and then the GP has the headache of restoring it. There are quite a few surgical specialists that need to realize that the standard of care is now restoratively driven and no longer surgically driven implant dentistry.
Winnie
Winnie,
'was great meeting you at Siroworld. I have a bunch of these unfortunately...
On 9/29/2017 at 1:44 pm, Dr. Alfred Josephsen said...Agree with above.
Any idea if the operator placed it as an immediate and just used the palatal socket ( thereby explaining the less than ideal positioning? )
Is that bleeding in the screw access?
If the patient was told by someone that his fixture was "ready for restoration" and then it fails subsequent to having been loaded by your restoration through no fault of yours or your beautifully performed restoration .... oh, boy... Hope not!
The bleeding occurred when I deformed the tissue placing the custom abutment, I tried to shape it as best as possible and slowly screw it to place.
I have no idea how it was placed.
one thing if it fails, it seems it is so far off I could remove it and place the new one in the proper position
Thanks
On 9/29/2017 at 1:45 pm, Charles LoGiudice said...Very nice save.
Thanks!
Was also great meeting you at Siroworld
On 9/29/2017 at 3:35 pm, Robert Lang said...On 9/29/2017 at 1:26 pm, Askold Wynnykiw said...On 9/29/2017 at 12:49 pm, David Sullivan said...Nicely done! Did you by any chance try to probe around the implant? The x-ray looks suspicious to me. Add to that the deep placement, yet the cover screw is exposed and the purplish looking tissue around the implant and I am wondering if there is already 50% bone loss on this fixture. The DB root (and maybe a smidge of the MB) still appear to be in the bone with grafting material placed on top. I may be wrong!!
I was wondering the same thing....
Unfortunately, this is a far too common occurence..... The dentist/specialist places the implant and then the GP has the headache of restoring it. There are quite a few surgical specialists that need to realize that the standard of care is now restoratively driven and no longer surgically driven implant dentistry.
Winnie
Winnie,
'was great meeting you at Siroworld. I have a bunch of these unfortunately...
Robert:
It was great meeting you as well !
Winnie
On 9/29/2017 at 3:34 pm, Robert Lang said...David and Leon
Exactly, I spoke to the patient and have major concerns. Did not probe, but still wondered if it would unscrew. I really leaned on it and was surprised it was solid, still informed the patient of my concerns.
I am at a quandary at times as I am just a country dentist and find it hard to send people back to the specialist.....
Your restoration looks great. As long as you informed the pt about the situation and they understand the risks and alternate options... then I think you are completely fine restoring and that it's the best possible result considering the situation.
My guess as to how this happened is that the surgeon did extraction and immediate placement. Placed the implant in the furcal bone and erred too far to the palate which explains why it's too distal, why it's too palatal, and why it's pretty deep. And then grafted and probably did something like put a collaplug on top (which doesn't work for well molars)... and then took a final x-ray and either didn't notice or didn't care that root tips were left. The tip of the implant is well integrated into the cortical floor of the sinus, but the top half is at high risk for peri-implantitis down the road.
In my short reply, I need to emphasize, considering the placement, that restoration is really great.
Robert-
From a Cerec perspective, nicely done. ![]()
As others have pointed our, upon evaluation of your x-ray, it looks like there may be less than ideal integration of the bone around the Implant.
To me, this case brings up the question of "What is a successful Implant?"
In my mind, an Implant should last at least ten years, preferably twenty and more. I think of a successful Implant as not just solidly in the bone, but part of a healthy Implant/Bone/Periodontal complex. If there is inadequate periodontal support around the crest of the Implant, threads will become exposed, bacteria will infiltrate, and over time, bone will be destroyed and the Implant will be lost within a few years. If there is partial integration, the same scenario is likely. I cannot know for certain how long this Implant will last, based on one x-ray, however, it would be interesting to look more critically. I think periodontal probing would be indicated. Possibly reverse torque testing to 35NCm.
You have done a very good restoration on a shaky foundation. I sincerely hope it works out well for you and your patient.
Jay
On 9/29/2017 at 9:35 pm, Jay Stockdale said...Robert-
From a Cerec perspective, nicely done.
As others have pointed our, upon evaluation of your x-ray, it looks like there may be less than ideal integration of the bone around the Implant.
To me, this case brings up the question of "What is a successful Implant?"
In my mind, an Implant should last at least ten years, preferably twenty and more. I think of a successful Implant as not just solidly in the bone, but part of a healthy Implant/Bone/Periodontal complex. If there is inadequate periodontal support around the crest of the Implant, threads will become exposed, bacteria will infiltrate, and over time, bone will be destroyed and the Implant will be lost within a few years. If there is partial integration, the same scenario is likely. I cannot know for certain how long this Implant will last, based on one x-ray, however, it would be interesting to look more critically. I think periodontal probing would be indicated. Possibly reverse torque testing to 35NCm.
You have done a very good restoration on a shaky foundation. I sincerely hope it works out well for you and your patient.
Jay
Jay,
i did probe, my wording preciously was poor. One of the reasons I put this here was for,discussion. I have had so many cases lately post ortho for implants and post implant show,up as new patients. I am struggling as to how to approach talking to specialists. One orthodontist said I was clueless (to the patient) about implants after he sent me a case for a lateral where the central and cuspid roots apically were almost,touching. It's funny if that was my implant it would be gone but yet in this case I tried to make it work. I always say I do,what's best for my patients but it appears I may have come up short here.
What do you guys do when you get cases like this from specialists?
Also this is a great forum for learning, it's hard to put your self out there and post cases. In other forums this discussion would not be as supportive...
Robert-
Great points for discussion. Situations like this can put us in a difficult situation as restoring dentists. I had a new patient present for restoration of an "All-on-X" (Don't remember the exact number of Implants.) a little over a year ago. Some were solid, but several were very questionable. My recommendation was to remove the questionable ones, replace them, then restore. I reviewed the CBCT with the patient thoroughly, to explain why I was making that recommendation. Obviously, this is not what any patient wants to hear, and I certainly sympathize with them. After a cordial visit, the patient left and I have not seen them since.
I am OK with that.
Patient was informed of their situation and made their decision accordingly. I recommended what I felt was in the patient's best long term interests. While it was not enjoyable losing out on the production for a large case, I was imagining the problems I would be getting into if I restored the case and then it failed. In your case, you are essentially rolling the dice, hoping the Implant will not fail. Again, I sincerely hope that it does survive. I do not know the laws in your state, but in California, we have the option to decline to treat. I have used this option numerous times over the years, and am comfortable with that.
This case is a great example of real world challenges that we, as general dentists, can routinely face. I appreciate you posting a difficult situation and allowing us to comment on it.
Jay
Great post and discussion points all around. It makes me feel so good to be a part of this exceptional group. Thanks everyone!
If you think that implant was bad you should check into some lab forums. Maybe you are in another phase of your life and can afford to dump cases. Over here work is work and yes the implant is not ideal but its integrated and has the screwy side up....
Jay,
Thanks for the comments, I just need to say no. Which obviously is hard for me to do.
A wise man once told me "it is better to see the back of their heads one time then their face over and over"
Robert-
Will be interesting to see how this works out in the future. ![]()
@Jos-
As I see it there are two issues here:
1 - What is in the best long term interests of our patients.
2 - What is in our own financial interests.
For me, these are not opposing issues. To restore questionable Implants that come our way can result in creating significant problems for our patients, and financial problems for ourselves. If I had restored the All-on-X case and it failed, that would create a big problem in my patient's life, and likely, a big financial problem for me. Not just in direct reimbursal, which patients tend to demand, but time.
Time.
As others have repeatedly noted, time is all we have to exchange for revenue in our practices. Fiddling with redos and replacements is a huge time waster. I am as keen to generate production as you are. My strategy to that end is to avoid redoing treatment as much as possible. The cost of redoing one case negates the profit from several successful cases. All of us have our own strategies in regards to this. This reminds me of a saying my Dad told me a long time ago:
"There are old pilots and there are bold pilots, but there are no old, bold pilots."
Jay
On 10/1/2017 at 9:01 am, Jay Stockdale said...Robert-
Will be interesting to see how this works out in the future.
@Jos-
As I see it there are two issues here:
1 - What is in the best long term interests of our patients.
2 - What is in our own financial interests.
For me, these are not opposing issues. To restore questionable Implants that come our way can result in creating significant problems for our patients, and financial problems for ourselves. If I had restored the All-on-X case and it failed, that would create a big problem in my patient's life, and likely, a big financial problem for me. Not just in direct reimbursal, which patients tend to demand, but time.
Time.
As others have repeatedly noted, time is all we have to exchange for revenue in our practices. Fiddling with redos and replacements is a huge time waster. I am as keen to generate production as you are. My strategy to that end is to avoid redoing treatment as much as possible. The cost of redoing one case negates the profit from several successful cases. All of us have our own strategies in regards to this. This reminds me of a saying my Dad told me a long time ago:
"There are old pilots and there are bold pilots, but there are no old, bold pilots."
Jay
Love that quote
I did want to chime in on the part about reaching specialists.
I appreciate that someone took the time and effort to try to reach out to me (Winnie and Gene).
I know it won't be easy, but find someone who will honestly sit down and go over these cases in a professional manner.
It might take a few tries to get the right person, but it's worth it to have someone who you can bounce cases off of (mutually).
The two GPs who woke me up couldn't be more different, yet I respect them both so much for what they did.
Gene Messenger has a huge practice and does a lot of his own implant placements, and we have had a lot of great conversations about cases he's done.
Winnie has a small boutique practice, doesn't do any surgery, is one of the best restorative dentists I've ever worked with, and I have learned so much about treatment planning and sequencing from him.
Hopefully, I've helped them understand how I look at cases as an Oral Surgeon with 25 years of experience.
Just my two cents...
As far as the case goes, the implant is too short as well. I have seen these cases improve over time as long as hygiene is good and occlusion is controlled. The grafting at the crestal portion can and usually does eventually turn over into bone. Keep them away from almonds and popcorn!
On 10/2/2017 at 4:05 am, Douglas Smail, OMFS said...I did want to chime in on the part about reaching specialists.
I appreciate that someone took the time and effort to try to reach out to me (Winnie and Gene).
I know it won't be easy, but find someone who will honestly sit down and go over these cases in a professional manner.
It might take a few tries to get the right person, but it's worth it to have someone who you can bounce cases off of (mutually).
The two GPs who woke me up couldn't be more different, yet I respect them both so much for what they did.
Gene Messenger has a huge practice and does a lot of his own implant placements, and we have had a lot of great conversations about cases he's done.
Winnie has a small boutique practice, doesn't do any surgery, is one of the best restorative dentists I've ever worked with, and I have learned so much about treatment planning and sequencing from him.
Hopefully, I've helped them understand how I look at cases as an Oral Surgeon with 25 years of experience.
Just my two cents...
As far as the case goes, the implant is too short as well. I have seen these cases improve over time as long as hygiene is good and occlusion is controlled. The grafting at the crestal portion can and usually does eventually turn over into bone. Keep them away from almonds and popcorn!
This is what it's all about. Congrats to Doug, Gene, and Winnie for striving to optimize patient care through communication and a common goal.
On 10/2/2017 at 4:05 am, Douglas Smail, OMFS said...I did want to chime in on the part about reaching specialists.
I appreciate that someone took the time and effort to try to reach out to me (Winnie and Gene).
I know it won't be easy, but find someone who will honestly sit down and go over these cases in a professional manner.
It might take a few tries to get the right person, but it's worth it to have someone who you can bounce cases off of (mutually).
The two GPs who woke me up couldn't be more different, yet I respect them both so much for what they did.
Gene Messenger has a huge practice and does a lot of his own implant placements, and we have had a lot of great conversations about cases he's done.
Winnie has a small boutique practice, doesn't do any surgery, is one of the best restorative dentists I've ever worked with, and I have learned so much about treatment planning and sequencing from him.
Hopefully, I've helped them understand how I look at cases as an Oral Surgeon with 25 years of experience.
Just my two cents...
As far as the case goes, the implant is too short as well. I have seen these cases improve over time as long as hygiene is good and occlusion is controlled. The grafting at the crestal portion can and usually does eventually turn over into bone. Keep them away from almonds and popcorn!
Doug,
Thanks for the comments, its all about communication and this forum here is great for that. Everyones willingness to contribute and share and not bash the presenter, In this case me...
Thanks again for all the comments
Doug, as a user of Bicon implants, I'm thinking the length of the implant is plenty long but a wider implant such as a 6.0 would be beneficial... so maybe a 6.0X5.0, guided of course, as a guess without having the CBCT.
Karl Schneck