Onlays with open margins
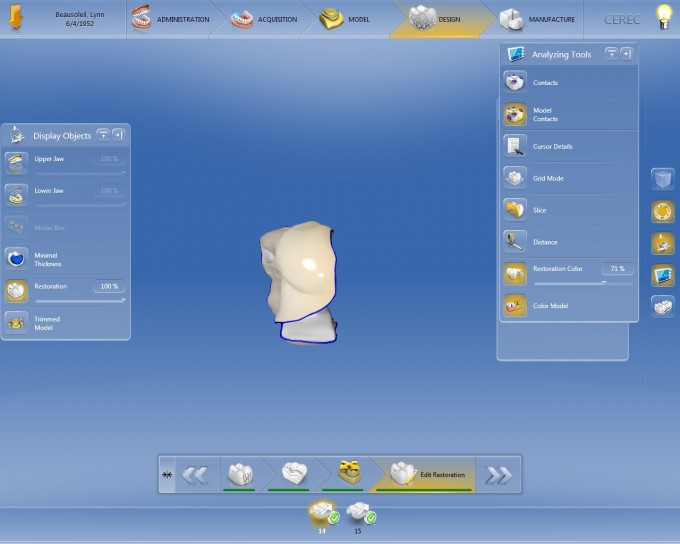
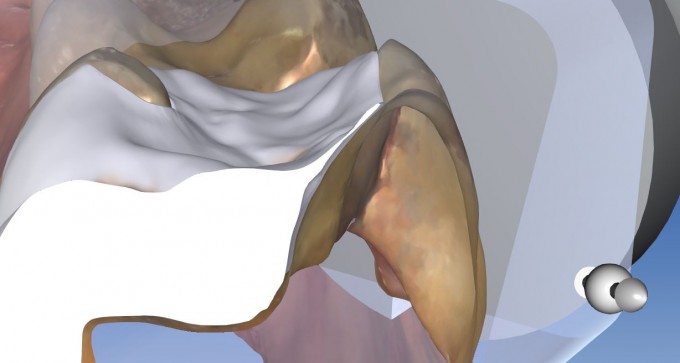
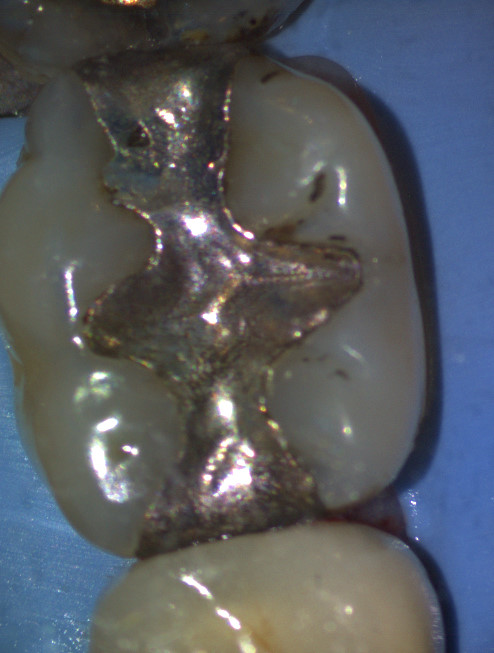
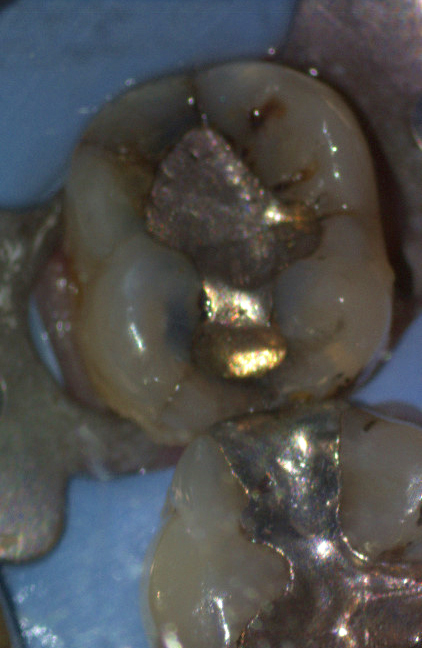
Here is a recent case I did. I'm noticing that my margins aren't closed when I do these cases. Does anything stand out as a possible reason for this? I thought my paramters were corect. See attached photos for final product. In retrospect, I should have prepped out the rest of the remaining lingual structure. 


I do a lot of onlays and I have this problem once in a while. There are three reasons for this issue: interproximal contacts that are too tight, undercuts in the preparation, and sharp line angles in the preparation instead of rounded line angles--or a combination of all three. The problem with undercuts in the preparation is that sometimes they matter and sometimes they don't. Inlays and onlays are the most difficult CEREC procedures we do and I think that it is nearly impossible to not encounter this problem occasionally. I have observed that as I do more of them--ie. get more experience--my success rate has improved. Sometimes it is necessary to accept "an island of milled composite in a sea of bonding resin or flowable composite" and move on. Since we are not using zinc phosphate cement, these things normally look OK on recall since the bonding resin is essentially the same material as the inlay/onlay.
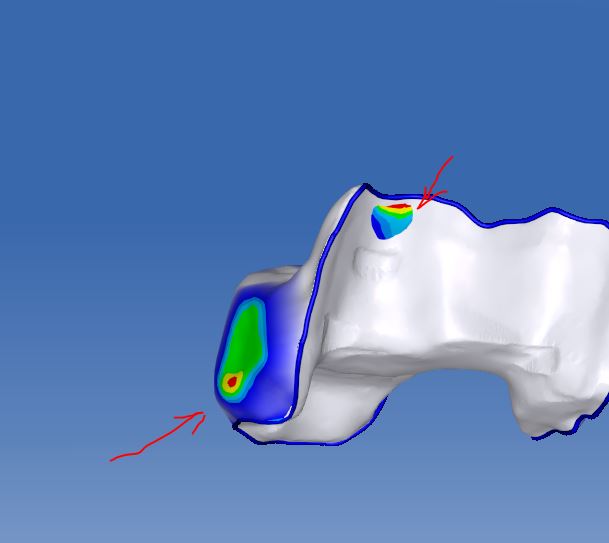
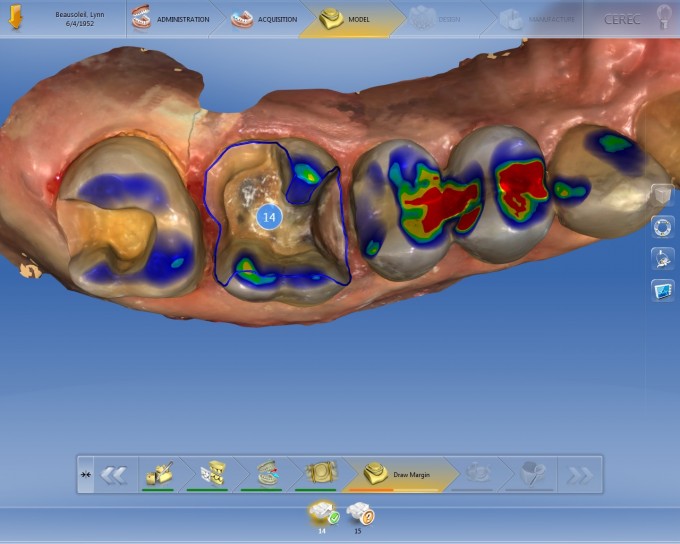 I think your radius on transitions are a little tight
I think your radius on transitions are a little tight
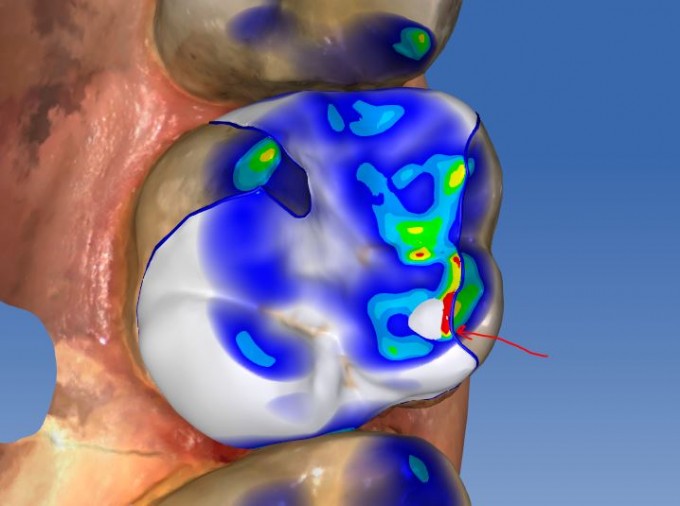
Your margin is in an area where you have occlusal contact
thin area on occlusal margin area that may be affecting mill/ seating
a step in margin on mesial that leaves a possible point of binding
proximal surfaces on proposals have concave areas- I think contacts is main culprit but all can add up to seating issues Turn contacts off in analysing tools to se true surface w/o colors
prep on 15 is a much more cerec friendly prep
...always polish adjacent contact areas. The bi is pretty rough looking.
...never save a cusp sliver. It becomes a liability.
...the full coverage onlay (crownlay) is a much better restoration.
I do a ton of onlays. It is rare that they just drop in. I use a piece of red, single sided accufilm to find impingement areas on the intaglio and the contact areas. Usually it takes three adjustment tryins to make it fit perfect.
Agree... internal restorations are the most difficult both prepping, seating, and often do not hold up well in ceramics esp if cusp inclines are steep, and occlusal wear/contact areas. I'm not sure the restoration is completely seated in photo... there's a potential binding area on MB internal wall, as well as the distal contact contour built into the adjacent undercut
Once those have been adjusted, and it is in fact seated without proximal contact interference or internal binding there is the main problem of very thin porcelain being milled, that I would expect significant chipping, as well as an actual penetration of the internal of the restoration below your margin line (showing thru the restoration both in design and in the mill)
Once you've got it seated, and having lost that part of the restoration, your gap will be at least the dimension of your spacer parameter...
Agree with Brian--- these thin cusps are an actual long term liability, aside for the added complexity to designing and milling the restoration. In the 1st molar restoration, just a cusp reduction, and smoothing transitions would make this drop in without a sweat, and will last much better... when we DO these restorations, with cavosurface margins, I think the hybrid materials not only mill cleaner, but last much better in function....Did a LOT of these type of designs, in pre-3d days, and resin cements will fill the gap and do well enough, but it's not as predictable and durable.....just have to get over the paradigm that in trying to be "conservative" in the best interests of the patient, that reducing the cusps really does serve everyone involved better--- you and the patient. Hope that helps.
Mark
Thank you for your feedback! Contacts were the first thing I checked and I actually ended up slightly over reducing them during polishing to see if it would help (it did not). I definitely will need to improve my prep design.
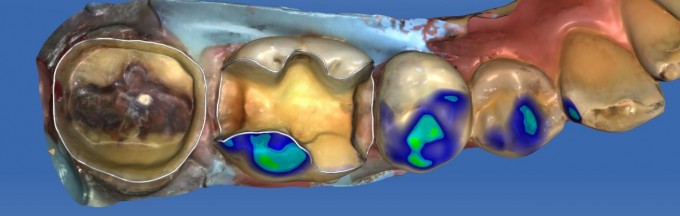
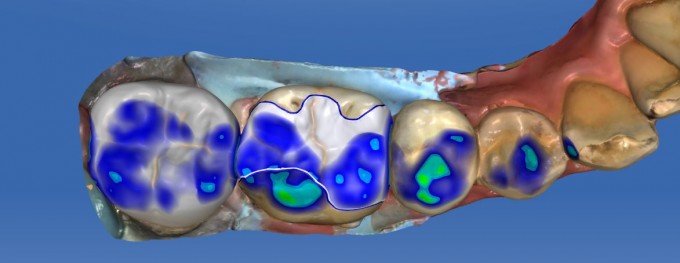
Hi Arash- thought I would follow up with a recent case that "might" address your respectable desire to be conservative, and and example of when I might cover a cusp or leave it... usually on molars, if there is an MOD present, I'm more likely to cover the cusps than leave them, but at least in a few recent cases made the decision to leave some intact..
30 existing MOD-A, recurrent caries apparent MB cusp
31 O-A recurrent caries multiple fracture present, remarkable asymptomatic
Removed amalgams initially with depth bur, just to establish fissure depth adequate for e.Max (1.5mm depth bur) on 30... 1.0 on 31 appropriate for Zirconia
Was pretty committed to circumferential coverage of 31 just based on clinical appearance, and in a less esthetic area felt that zirconia would be my choice in a "conservative" mind to reduce less occlusally and axially... Extending only enough for proper resistance and retention form for a conventionally cemented restoration, to include fractures as much as possible. On 30, there was recurrent caries as anticipated undermining MB cusp, but the rest was clean.... at which point its a game time decision to reduce remaining cusps or not... in this case I didn't. Spefic reason? Complete vertical functioning patient, no fractures, dentin supported cusps, and esp not a lot of complexity that would complicate the seating... and because there are cavosurface margins, I felt a hybrid would wear and function better marginally (used Cerasmart). There was still some minor contact at DB margin, but the hybrid wears better, AND I adjusted opposing lightly to remove that area only...
If I had decided I needed to cover the cusps which what was suggested above in one of your case examples...I would have taken what I had here in the design pic, and just reduce the remaining cusps sufficiently for the material (complete occlusal coverage would have been e.Max) and just smooth/blended the transitions from proximals to buccal and lingual surfaces... make sure there is at least a semi-functional cusp bevel buccally--- which is not a resistance/retention form issue as it is a sufficient thickness material for the case. More examples could be given, but was just trying to show that it's not dogmatic about not leaving cusps, it just depends on the case. Making your cases easier and more predictable, also makes you a better dentist. :)
Not to beat a dead horse, but being conservative means different things to different people. But as far as how I think about it, I'd rather not leave things subject to predicable fracture, have restorations that are predictably delivered, and that means enough occlusal reduction---where there is plenty of enamel to bond to.... I am more concerned about reduction nearer the CEJ where you are closer to pulp space, cutting away enamel to bond to, expose pt to easier recurrent decay potential, etc. More could be said about all of that, but a good video series is available with better information.....
Hope that helps!
Mark