Digital Magazine
Digital Magazine
Digital Magazine
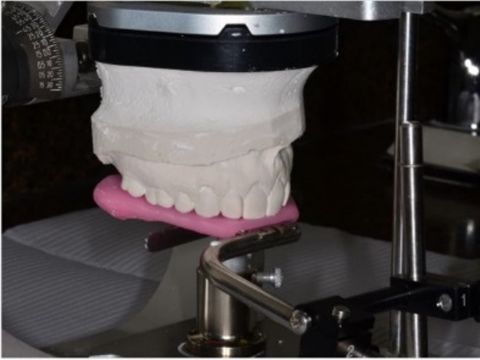
Determining Vertical Dimension for Worn Dentition Case
Digital Magazine
The Chairside Zirconia Revolution: The Evolution of Choice
Announcements and Feedback
New Dates Added
Digital Magazine
New Technologies and 3D Imaging — “The Virtual Microscope”
Digital Magazine
These Workshops Changed the Way I Look at Teeth
Announcements and Feedback
My 15-Year Journey With Lithium Disilicate
Announcements and Feedback
Rediscovering a Passion for Dentistry
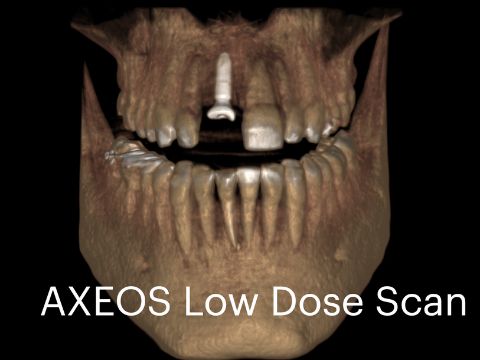
Cone Beam and Implants
CBCT Shines a Light on Every Day Diagnosing and Treatment Planning
Announcements and Feedback
Improving Patient Communication
Announcements and Feedback



 By Farhad Boltchi, D.M.D.
By Farhad Boltchi, D.M.D.

 By Mike Skramstad
By Mike Skramstad

 By CDOCS Staff
By CDOCS Staff


 By Diwakar Kinra
By Diwakar Kinra