Digital Magazine
Digital Magazine
Announcements and Feedback
The Vantage Point: Free Virtual Seminar
Digital Magazine
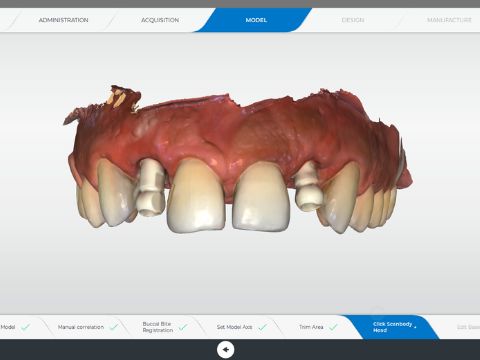
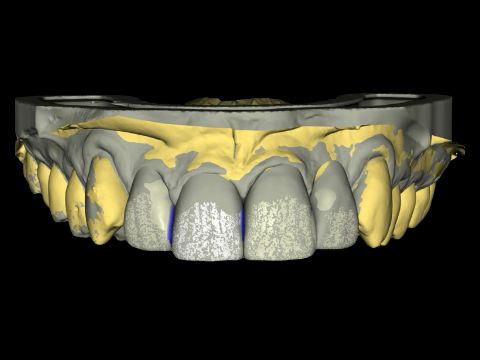
Restoring Implant Bridges with CEREC® and Atlantis
Digital Magazine
Versatility in the CEREC® World Today
Digital Magazine
Orthodontics and CEREC ®
Digital Magazine
Sometimes We Just Can’t Be Ideal
Announcements and Feedback
Join us on the CDOCS Summer $500 Tour
Digital Magazine
New Infrastructure Needed, Bridge Replacement
Digital Magazine
Knowing More About Photo-Chemical Etching
Digital Magazine
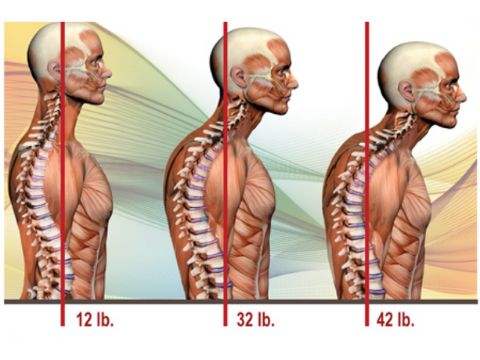
8 Exercises to Ease That Dental-Related Neck and Back Pain
Digital Magazine
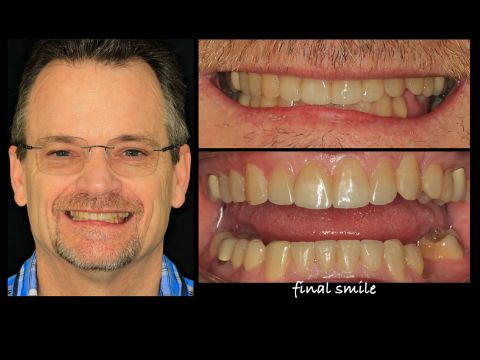
Interdisciplinary Case Report
Announcements and Feedback



 By Dhaval Patel
By Dhaval Patel

 By CDOCS Staff
By CDOCS Staff

 By Dan Butterman
By Dan Butterman

 By Kristine Aadland
By Kristine Aadland
 By Ross Enfinger
By Ross Enfinger
 By Meena Barsoum
By Meena Barsoum



 By John Hamlin
By John Hamlin
 By Darin O'Bryan
By Darin O'Bryan