General Discussion
Digital Magazine
Digital Magazine
Extra Fine Milling Katana STML
Digital Magazine
Dentsply Sirona World 2021
Digital Magazine
Staged Transcrestal Sinus Lift: An Alternative Approach
Digital Magazine
What Lies Beneath the Surface?
Digital Magazine
The Y’s of Zirconia
Digital Magazine
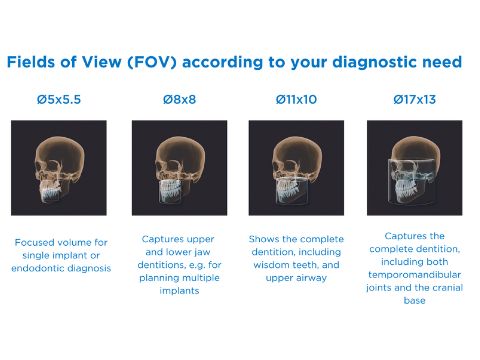
Axeos: Favored by Dentists, Loved by Patients
Digital Magazine
Copy And Mirror Is Ideal For Single Centrals
Digital Magazine
CERASMART® 270 and G-CEM ONE™- A Winning Combination
Digital Magazine
Why I Use LendingClub Patient Solutions
Announcements and Feedback
Dentsply Sirona World is BACK in Las Vegas!
Digital Magazine



 By Sean Clark-Weis
By Sean Clark-Weis

 By Mike Skramstad
By Mike Skramstad

 By CDOCS Staff
By CDOCS Staff

 By Farhad Boltchi, D.M.D.
By Farhad Boltchi, D.M.D.

 By Karyn Halpern
By Karyn Halpern


 By Meena Barsoum
By Meena Barsoum



 By Anthony Ramirez
By Anthony Ramirez